Credentialing
Simple step by step credentialing with Complete Practice Solutions
We Can SIMPLIFY The Process of Credentialing
Managing a medical practice in today’s fast-paced environment can present payment issues far beyond the scope of your practice manager’s expertise to successfully resolve. Consistent results require a team of specialists with the experience and skills to cut through red tape. Let our team of experts resolve your credentialing and contracting issues.
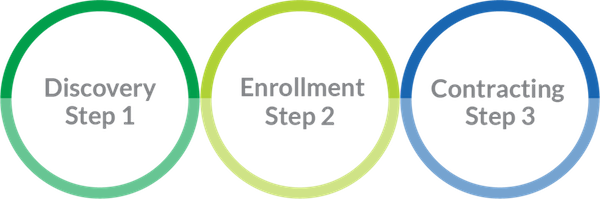
Discovery
• Gather provider and/or group information
• Account Setup
• CAQH Review – Update – Setup
• Review Current Plan Enrollments
• Determine Plans and Enrollment type
Enrollment
• Contact Insurance payers
• Prepare and Submit Enrollments
• Follow up on submissions until approval/denial
• Provide regular updates
Contracting
• Verify all contracts are signed and executed
• Verify Network participation status
• Verify start date
Credentialing Simplicity
Each provider or group organization has their own unique set of circumstances. Are you a new provider just starting out, or an established practice adding a new provider to your existing group? Are you relocating to another state to practice or rendering services in multiple states? Whatever your current scenario, let our knowledgeable team simplify the complex process of credentialing, freeing you and your staff to focus on what you do best.
Package Flexibility
We credential groups, individual providers, and mid-level practitioners, offering packages based on the number of payors, providers and groups selected.
Demographic Updates
As your practice grows and changes, insurance companies require current records. Adding a new location or provider means that your existing contracts need to be updated to reflect those changes. Incorrect demographic information can lead to termination of an existing contract or claims being rejected.
Credentialing FAQs
The enrollment options are as follows: Individual, Group, Medicare, Medi-Cal and Medicaid.
Each individual provider will need to complete the 3-step credentialing process. Once the credentialing process is complete, the individual provider will be considered an “in network” or “participating” provider.
Group enrollment uses your legal business name and group tax id. A group contract is required for you to submit claims using that business name and tax id and requires similar steps as individual enrollment.
In order to submit claims using the group contract, individual providers must be credentialed and linked to the group.
Until a provider has completed the credentialing process for each insurance company they choose to work with, claims submitted will be rejected or paid as out of network.
Each valued customer is provided a client log in to a secure platform, offering a safe place to store sensitive provider information.
Change of Address
Change of Ownership
Adding a New Location
Adding Existing Provider to Practice
Removing Termed Provider from Contract
New Phone or Fax Number
Individual Enrollment
Group Enrollment
Reassignments
Re-Validation
Demographic Updates